Diabetes research at Whitehead Institute
This story is part of our series, An energetic pursuit. Click here to see all stories in this collection.
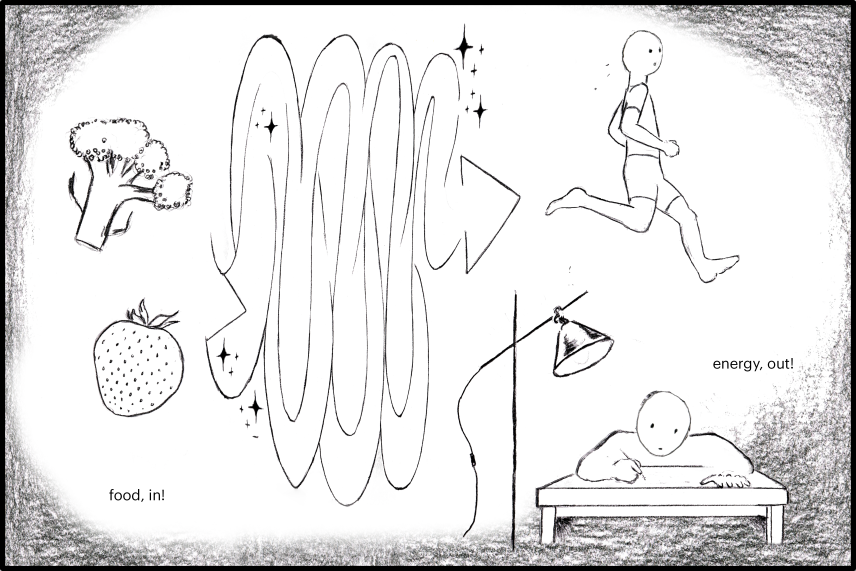
Diabetes is a disease of our metabolism, how our bodies convert food into energy. Food gives us the ability to move, to think, and to keep our bodies functioning.
Madeleine Turner/Whitehead Institute
Madeleine Turner/Whitehead Institute
To understand diabetes, it's helpful to look at the process of converting food into energy.
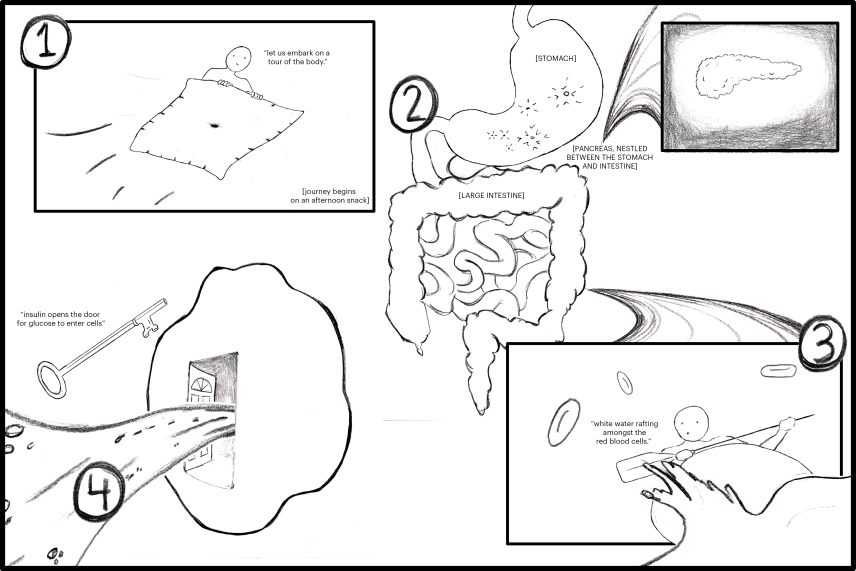
When food enters our stomachs, our stomachs break down carbohydrates into a simple sugar, called glucose.
Glucose travels to the intestines, where it's absorbed into the bloodstream. It's on a journey through the bloodstream to reach all types of cells throughout the body, where it can be converted into energy. Glucose can't enter cells on its own. It needs the "key" to access cells, the hormone insulin.
The pancreas, nestled between the stomach and large intestines, produces insulin according to how much glucose is flowing in the bloodstream at a given time. Diabetes can happen when the body can't make insulin, can't respond to insulin, or a combination of the two.
Madeleine Turner/Whitehead Institute
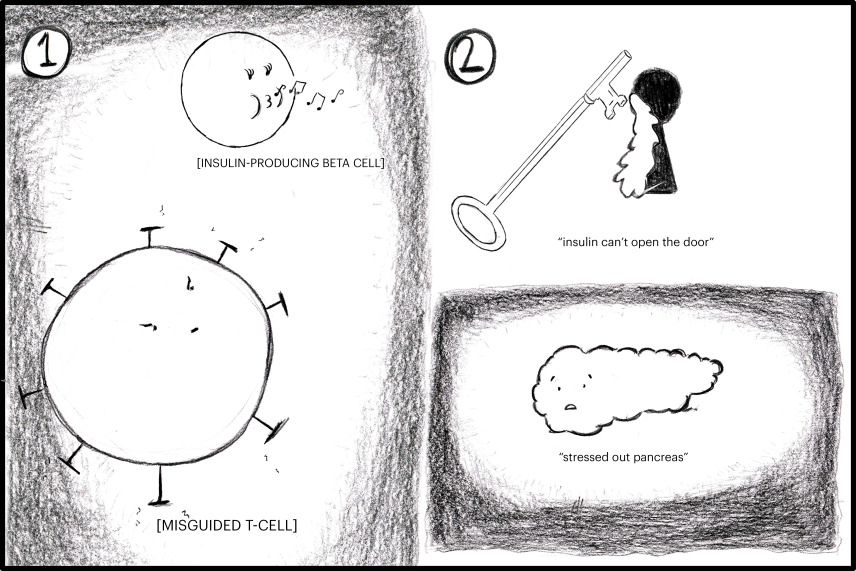
- Type I diabetes is an autoimmune disease. In this form of the disease, the body's immune system mistakenly attacks beta cells, which produce insulin in the pancreas.
- In contrast to Type I, Type II diabetes usually appears later in life. In this form of the disease, multiple systems slowly fail over time. In some cases, a person with Type II diabetes can produce insulin as normal. But cells have trouble responding to that insulin correctly, meaning the body cannot use or store sugar from food. Sometimes, the pancreas sends out an increasing amount of insulin to compensate, until the pancreas wears out.
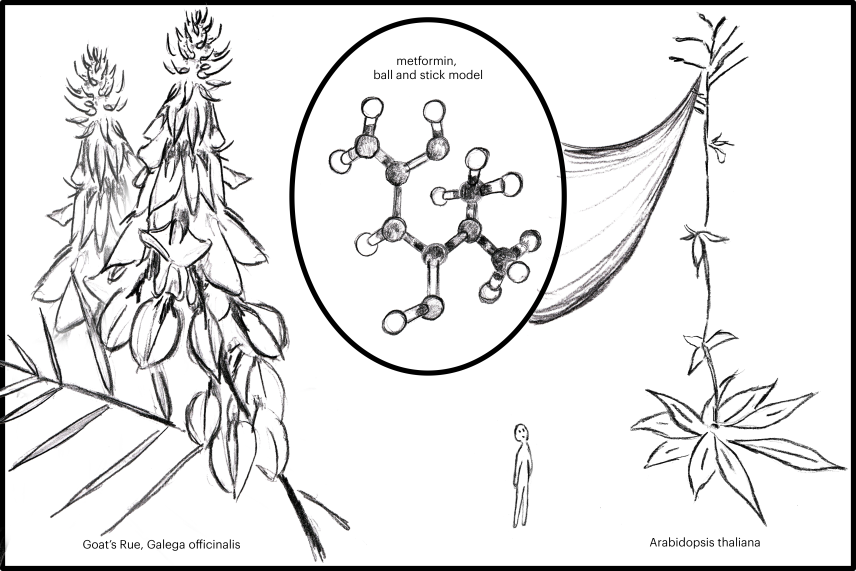
Two labs at Whitehead Institute study metformin, a drug administered to Type II diabetes patients. The drug has multiple effects: it can spike cell sensitivity to insulin, and it can curb how much sugar is introduced to the bloodstream, in both the liver and intestines.
Madeleine Turner/Whitehead Institute
Galega officinalis, or goat's rue, had been used over several centuries to treat diabetes, long before metformin became a go-to treatment. The plant's therapeutic effect comes from galegine, a compound with a structure similar to metformin.
Whitehead Institute Member Jing-Ke Weng strives to understand how this compound is synthesized in goat's rue. Weng's lab also studies how metformin impacts metabolism in plants, using Arabidopsis thaliana as a model.
The second lab to study metformin at Whitehead Institute is Richard Young's lab. Alessandra Dall’Agnese, a postdoc in the lab, studies this diabetes drug in the context of condensates.
Madeleine Turner/Whitehead Institute
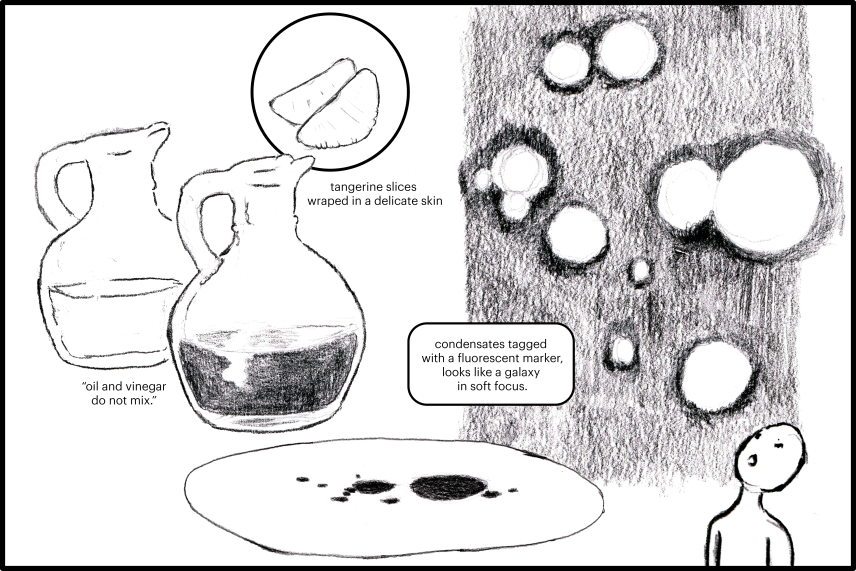
What is a condensate? In high school biology, one might learn about organelles, which are structures in the cell that perform specialized tasks and are held together by membranes — sort of like the delicate skin of a tangerine holding in its juices. The word literally means "little organs."
In contrast, condensates are cellular structures held together without any membrane. These tiny droplets within the cell form due to a process called phase separation, which is similar to how vinegar evades being mixed with oil, instead pooling on its own.
In the past, researchers in Young's lab focused on how various cancer drugs concentrated within condensates, and how this property could affect the delivery of the drug. Dall'Agnese is now taking a similar approach to study how metformin interacts with condensates.
Researchers at Whitehead Institute also study mechanisms contributing to diabetes.
Madeleine Turner/Whitehead Institute
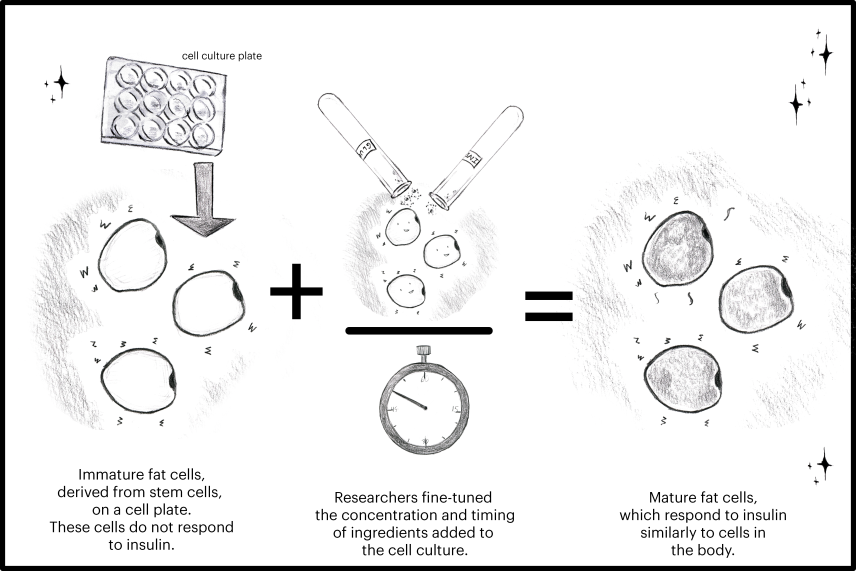
Whitehead Institute Member Rudolph Jaenisch and postdoc Haiting Ma engineer cells in the lab to recreate what happens inside a human pancreas. Their work involves simulating a complex piece of biology in a controlled setting. They program stem cells to become T cells and Beta cells, recreating an autoimmune response inside a Petri dish.
Other researchers in Jaenisch's lab work on recreating diabetes in a dish. Postdoc Max Friesen, for example, uses stem cells to model the function of liver and fat cells in the context of diabetes. In both projects, Haiting and Max focused on fine-tuning conditions of the cell culture, in order to develop mature differentiated cells that function similarly to cells inside the body.
Researchers at Whitehead Institute continue to study diabetes in hopes of improving therapeutics and maybe one day developing a cure.
Topics
Contact
Communications and Public Affairs
Phone: 617-452-4630
Email: newsroom@wi.mit.edu


