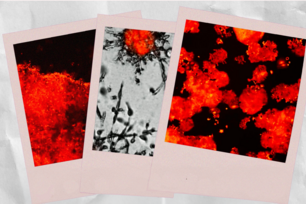
In this model of tumor ischemia, the outer region of the tumor has access to oxygen and nutrients from the host (DNA stained blue). Meanwhile, the central region of the tumor has limited access to the oxygen and nutrients, and undergoes massive cell death (red). Control (shGFP) glioma cells, which express high levels of SHMT2 (green), are able to partially survive the central ischemic region, as evidenced by the numerous patches of green and red stained cells. On the other hand, tumors from cells with SHMT2 knockdown have a central region that is devoid of surviving cells. The bottom panels are 8X magnifications of the central tumor region; blue nuclear stain is not shown, for clarity.
Courtesy of Nature.
Biologists identify brain tumor weakness
Biologists at Whitehead Institute and MIT have discovered a vulnerability of brain cancer cells that could be exploited to develop more-effective drugs against brain tumors.
The study, led by researchers from Whitehead and MIT’s Koch Institute for Integrative Cancer Research, found that a subset of glioblastoma tumor cells is dependent on a particular enzyme that breaks down the amino acid glycine. Without this enzyme, toxic metabolic byproducts build up inside the tumor cells, and they die.
Blocking this enzyme in glioblastoma cells could offer a new way to combat such tumors, says Dohoon Kim, a postdoc at Whitehead and lead author of the study, which appears in the April 8 online edition of Nature.
David Sabatini, a Whitehead Institute Member and professor of biology at MIT, is the paper’s senior author. Matthew Vander Heiden, the Eisen and Chang Career Development Associate Professor of Biology and a member of the Koch Institute, also contributed to the research, along with members of his lab.
GLDC caught the researchers’ attention as they investigated diseases known as “inborn errors of metabolism,” which occur when cells are missing certain metabolic enzymes. Many of these disorders specifically affect brain development; the most common of these is phenylketonuria, marked by an inability to break down the amino acid phenylalanine. Such patients must avoid eating phenylalanine to prevent problems such as intellectual disability and seizures.
Loss of GLDC produces a disorder called nonketotic hyperglycinemia, which causes glycine to build up in the brain and can lead to severe mental retardation. GLDC is also often overactive in certain cells of glioblastoma, the most common and most aggressive type of brain tumor found in humans.
The researchers found that GLDC, which breaks down the amino acid glycine, is overexpressed only in glioblastoma cells that also have high levels of a gene called SHMT2, which converts the amino acid serine into glycine. Those cells are so dependent on GLDC that when they lose it, they die.
Further investigation revealed that SHMT2 is expressed most highly in cancer cells that live in so-called ischemic regions — areas that are very low in oxygen and nutrients. These regions are often found at the center of tumors, which are inaccessible to blood vessels. It turns out that in this low-oxygen environment, SHMT2 gives cells a survival edge because it can indirectly influence the activity of an enzyme called PKM2, which is part of the cell’s machinery for breaking down glucose.
Regulation of PKM2 can impact whether cells can generate the material to build new cancer cells, but the same regulation also affects the consumption of oxygen — a scarce resource in ischemic regions.
“Cells that have high SHMT2 activity have low PKM2 activity, and consequently low oxygen-consumption rates, which makes them better suited to survive in the ischemic tumor microenvironment,” Kim says.
However, this highly active SHMT2 also produces a glut of glycine, which the cell must break down using GLDC. Without GLDC, glycine enters a different metabolic pathway that generates toxic products that accumulate and kill the cell.
“An interesting aspect of the current study is that they uncovered why glycine accumulation is toxic,” says Navdeep Chandel, a professor of medicine and cellular biology at Northwestern University who was not part of the research team. “GLDC loss accumulates glycine, causing nonketotic hyperglycinaemia, a disorder that severely affects the developing brain. Sabatini and colleagues elucidated that loss of GLDC builds up glycine levels, resulting in funneling of glycine into metabolic pathways that generate toxic molecules, such as aminoacetone and methylglyoxal.”
The finding also raises the possibility that these GLDC-dependent cells could be killed with drugs that block GLDC activity, according to the researchers, who are now seeking potential drug compounds that could do just that.
The research was funded by the American Brain Tumor Association, the National Institutes of Health, and the Koch Institute.
* * *
David Sabatini's primary affiliation is with Whitehead Institute for Biomedical Research, where his laboratory is located and all his research is conducted. He is also a Howard Hughes Medical Institute investigator and a professor of biology at Massachusetts Institute of Technology.
* * *
Kim, D., Fiske, B. P., Birsoy, K., Freinkman, E., Kami, K., Possemato, R. L., . . . Sabatini, D. M. (2015). SHMT2 drives glioma cell survival in ischaemia but imposes a dependence on glycine clearance. Nature, 520(7547), 363-367. doi:10.1038/nature14363
Topics
Contact
Communications and Public Affairs
Phone: 617-452-4630
Email: newsroom@wi.mit.edu