Gretchen Ertl/ Whitehead Institute
Harnessing the immune system to fight cancer
Sometimes research takes scientists to unexpected places, even alpaca farms. Tobiloba Oni is one of two Valhalla Fellows at Whitehead Institute who are researching ways to harness our natural defenses to combat cancer, an approach called immunotherapy. Oni found himself at an alpaca farm last summer not to admire the alpacas' fluffy coats and endearing underbites, but to draw blood. In the alpaca blood, Oni hopes to discover antibodies that may recognize and bind to pancreatic cancer cells.
Antibodies are proteins in the blood created to recognize specific molecules, called antigens, that are unique to a pathogen or other threats to the body. Part of Oni's research focuses on understanding how antibodies may be used to disarm cancer cells.
In a laboratory down the hall from Oni at Whitehead Institute, Valhalla Fellow Kipp Weiskopf explores the potential of immunotherapy for several challenging types of cancer, including lung cancer. Weiskopf looks to another component of the immune system, cells called macrophages.
Macrophages are large cells that engulf pathogens whole. These immune cells rely on "don't eat me" signals, such as the protein CD47, to avoid eating cells that are not pathogens. Many cancer cells also produce signals such as CD47, to evade an immune response. Weiskopf hopes to find ways to redirect macrophages, so that "don't eat me" signals in cancer cells do spark an immune response.
Both Oni and Weiskopf are seeking to understand how cancer cells dodge our bodies' natural defenses—research that may one day lead to new therapies that empower our immune response to attack cancer.
Tough like an oatmeal cookie
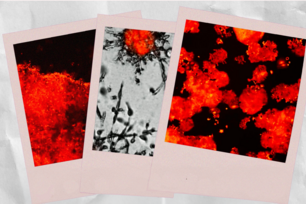
Pancreatic cancer is sometimes described by researchers as an oatmeal cookie. A solid mass might only be 20% cancer cells—the raisins—while the rest of the tumor is made up of non-cancerous cells, co-opted by the cancer for protection. Particular proteins dot the surface of cancer cells and allow cells to communicate with one another. Oni studies the network of cells and accompanying proteins that make up a tumor. Within this tumor microenvironment, Oni focuses on proteins found on cell surfaces, which can shield cancer from an immune response.
"We're trying to understand this critical interface in multiple ways," Oni says. "What are the key proteins that are educating the tumor microenvironment to prevent immune attack?"
Recently Oni has zeroed in on proteins called glycosyltransferases, which attach sugar molecules to proteins. By adding sugar molecules to other proteins on cancer cell surfaces, glycosyltransferases help pancreatic cancer cells evade an immune response. By experimentally removing glycosyltransferases, "you dramatically reshape that environment," Oni says. "Now the immune cells can attack pancreas cancers. In most cases, the tumors completely melt."
The lab continues to investigate how particular sugars equip cancer cells against immune attack, and how to disable this defense.
Glycosyltransferases are one of many lines of defense used by cancer cells. An array of proteins are found on the surface of pancreatic cancer cells, and are associated with the cancer's persistence. These proteins are not typically found on the cell surfaces of healthy cells. Oni’s lab is studying how targeting these cell surface proteins may increase the immune response.
"The cell surface is really the critical interface where the battle is happening," Oni says.
Turning cancer's friend to foe
Kipp Weiskopf is a Valhalla Fellow researching how macrophages, a type of white blood cell that consumes pathogens, function in tumor microenvironments. A goal of the Weiskopf lab is to develop therapies that take advantage of macrophages to attack cancer cells, with a focus on different types of metastatic cancer
"Within the setting of cancer, what we see is that macrophages at baseline tend to be suppressed, or they contribute to the growth of tumors. They actually do bad things within the tumor microenvironment," Weiskopf says.
This year Weiskopf and postdoc Dian Yang, a member of Whitehead Institute Member Jonathan Weissman’s lab, began developing a system to search for genes that can prompt macrophages to recognize and attack cancer cells. "We've identified a number of really exciting hits that we're investigating further in the laboratory," Weiskopf says.
In a parallel project, the Weiskopf lab is investigating whether particular drug cocktails can activate macrophages to destroy lung cancer cells, specifically drugs that block CD47, the "don't eat me" signal attached to cancer cells. "We've started to extend our findings to other types of cancer as well," Weiskopf says.
In other cases, it may be useful to turn down macrophage activation, like in the case of autoimmune disease, when our immune systems shift into overdrive.
"Are there other cells within the immune system that we can target? Cells…that may be more effective for some patients or for certain types of cancers, or maybe have a better safety profile in some settings?" Weiskopf says. "That's really where some of our work has grown."
Camelids are key
The Oni lab is interested not only in disrupting cancers' defenses, but also going on the offensive. An antibody is shaped like a Y, with the structure's top prongs having the ability to recognize and bind to specific antigens. In human antibodies, this "Y" shape is formed by two sets of polypeptide chains, with each set containing one heavy chain and one light chain. At the very top of the two prongs, each chain folds in on itself to create three protruding loops (called complementarity-determining regions, or CDRs) that stick out like fingers and can bind to an antigen. With a large surface area, most antibodies are limited in what they can bind to. "For example, if you have a small groove, the antibody cannot access it," Oni says.
Since human antibodies have limited capacity to bind to structures on cancer cell surfaces, Oni decided to look beyond our species. Camelids—a family that includes camels, llamas and alpacas—are known to produce a special type of antibody, called nanobodies. While camelid antibodies are also Y-shaped, they are missing light chains. Instead, a particular loop on each heavy chain is considerably longer, compared to the equivalent loop in most other antibodies. This elongated loop allows camelid antibodies to wedge into smaller crevices, tackling a greater number of threats.
(Sharks independently evolved the same solution and produce nanobodies. "But obviously, it's harder to do this research with sharks," Oni says. "Alpacas are kinder.")
By lucky coincidence, Oni connected with two Whitehead Institute donors who own an alpaca farm. Oni flew to California, and working with a veterinarian, took blood samples from twenty alpacas on the farm. Using the samples, Oni built an extensive library of heavy chain antibodies. The library is likely the largest of its kind.
The Oni lab is now studying the library to find alpaca antibodies that hit a sweet spot between binding to cancer cells, but not our own. The team combines nanobodies with conventional antibodies to uncover unique modifications that help shield pancreatic cancer cells. Oni also hopes to identify antibodies that can help guide an immune attack against cancer.
"We have the antibodies now," Oni says. "Hopefully we'll see some really exciting results."
Topics
Contact
Communications and Public Affairs
Phone: 617-452-4630
Email: newsroom@wi.mit.edu