Vaccine Technology Homes in on Cancer
CAMBRIDGE, Mass. — Science is based on novel, fascinating observations—most will remain a mystery, some may lead to a deeper understanding of life, but a few will lead to new therapeutic approaches to disease. Whitehead Member Richard Young is witnessing the impact of one such observation that he made about 15 years ago. His lab discovered a unique approach to vaccine development, which is now in phase III human clinical trials for the cancer-causing human papilloma virus.
"We started studying how the body’s immune system responds to tuberculosis and leprosy infections at Whitehead in the 1980’s. We discovered that about a half dozen proteins of these bacterial pathogens were specifically detected and targeted by the human immune system. Surprisingly, we found that they were all heat shock proteins," says Young. Many other laboratories began observing the same phenomenon in other bacterial, parasitic, and fungal infections.
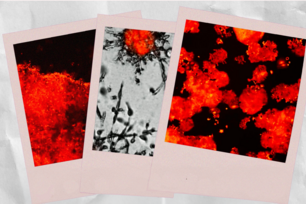
Heat shock proteins (HSPs), or stress proteins, are a family of proteins that cells produce in abundance in response to stress from heat, injury, or toxins. Normally these proteins act as molecular chaperones, binding to other proteins and ferrying them to and from various compartments of the cell. With infection, the bacterial heat shock proteins took on an additional role—they were a powerful stimulant of the human immune system.
Young, excited by the finding, embarked on the long road to understanding how HSPs trigger an immune response and how these results could be applied to vaccine development. His lab began to explore whether fusion of a HSP with an antigen of interest, such as a cancer antigen or a viral antigen not found in normal cells, might provide a new kind of vaccine.
An antigen is a piece of the virus or cancer cell that can be used to educate the immune system to target a specific virus or cancer cell. Immunologists knew that education of the immune system, however, also requires a stimulant that alerts the immune system to the presence of a foreign antigen. Young thought that an HSP-antigen fusion protein might provide a powerful combination of stimulant and antigen.
Vaccines Offer a Helping Hand
Vaccine development is a tricky proposition—produce a full-blown immune response that will protect the body without causing full-blown disease. Traditional vaccines used weakened or killed pathogens such as poliovirus. Scientists have since discovered that safer vaccines can be made in the lab. Instead of using a whole pathogen to trigger an immune response, a protein or sugar molecule from a bacteria or virus can accomplish the job if combined with appropriate immune system stimulants.
The goal of a vaccine is to trigger the two branches of the immune system. One branch, led by immune cells called B cells, produces specific molecules called antibodies into the body's fluids. These antibodies destroy the invading pathogen and keep vigilant watch for subsequent attacks. The second arm of the immune system, led by killer T cells or cytotoxic T cells, recognizes and destroys cells infected by pathogens or deformed by cancer. HSPs activate both arms of the immune system, even under the most difficult circumstances, when patients are immunocompromised as is the case with AIDS.
Young’s group made an additional observation suggesting that HSP vaccines might have both preventive and therapeutic properties. Mice immunized with HSP fusion proteins could be protected from certain cancers. Surprisingly, mice that already had cancer could be treated effectively with multiple doses of the HSP vaccine also.
Human Papilloma Virus Vaccine
Since the initial basic research studies, the HSP fusion technology has proven safe for use in human clinical trials conducted by Stressgen Biotechnologies, which licensed the technology from Whitehead. Stressgen and Roche have created a partnership to develop and commercialize a vaccine against human papilloma virus (HPV). The vaccine uses HSP fused with E7, a protein used by the human papilloma virus to stimulate neoplasias (precursors to cancer) and cancers.
HPV causes the most common sexually transmitted disease in the United States with 5.5 million new cases each year and often results in cervical and anal cancer. Positive results with small numbers of patients in phase II clinical trials make Young optimistic that the fusion protein approach actually works in humans.
"If the larger scale phase III clinical results are consistent with the phase II data, then we’ll have a new class of therapeutic. Even more importantly, the HSP fusion technology can be used to make a new generation of vaccines for protection and therapy against a broad spectrum of diseases," says Young.
Topics
Contact
Communications and Public Affairs
Phone: 617-452-4630
Email: newsroom@wi.mit.edu