Biography of a tumor
CAMBRIDGE, Mass. — It starts out just like every other cell. There’s nothing strange about it, no mutations, no odd behaviors—nothing that would distinguish it in any way from the countless cells with which it cohabits inside human tissue. Like all its neighbors, this cell multiplies only when it receives strict orders from its host tissue, and will stop the second it’s told. There is a fixed number of times the cell can divide, and once it has reached that limit, it will, as the poets say, shed its mortal coil.
This cell is such a team player that if it transgresses any of these barriers it will immediately commit suicide for the greater good of the organism, like a captured secret agent who pops a cyanide pill rather than divulge secrets to the enemy.
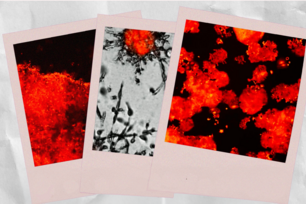
Over the years, however, this cell will sustain a mutation that sparks the development of a tumor mass, surpassing insurmountable odds in an exercise in Darwinian evolution that becomes the body’s nightmare. Just like the microscopic organism that slugged its way through primordial soup, evolving over billions of years into a creature capable of writing Hamlet and splitting atoms, this cell also will evolve, and over the course of a few decades, it will survive and grow and multiply in an environment so hostile, it’s amazing any tumor ever manages to survive.
Still, the life story of a tumor shows that ultimately, everyone is vulnerable to cancer. The human body comprises hundreds of billions of cells, and because many cells continue to divide throughout their lifetime, cancer remains a threat, however remote. In fact, many researchers believe that if we were spared death from all other diseases and lived virtuous lives complete with healthy diet and ample exercise, we all still would get cancer sooner or later, perhaps at age 170 rather than 70.
Tumors don’t develop overnight. Their growth is a long and arduous process that can take decades. To mature, tumors must circumvent a powerful biological defense system designed to kill the rogue cells that make up the mass. Not all tumors progress in exactly the same way. The stages may occur in a different order depending on the cancer, and the same type of cancer can progress quite differently from one patient to another. But there is a common script that most cancers follow, and while a person’s lifestyle choices certainly can enable a cancer’s progression, those stages occur mostly through the slow and random process of natural selection.
The biography of a tumor, then, is not a story about cancer’s prowess. It is about our vulnerability to random chance.
From humble beginnings
And so, we begin with an ordinary cell that lives harmoniously with its fellow cells somewhere deep inside the regions of a particular human tissue. Living harmoniously means, among other things, that there exists a perfect equilibrium between cell births and cell deaths. The cell will divide, birthing a replicate, or clone, of itself, only when another cell has died. Its genetic wiring ensures this.
However, when the cell divides and makes a copy of itself, it’s never a perfect replica. Each time, a miniscule mutation, sometimes only an alteration in a single letter of DNA, alters the new cell’s genome ever so slightly. In addition, toxins that enter the human body from, say, cigarette smoke, charred meat, or pollution, often affect some of the genes in this and other cells. In his book, One Renegade Cell, Whitehead Founding Member Robert Weinberg writes, “the genome of the human cell is constantly under attack, pelted by a hailstorm of damaging chemicals.” This happens all the time, and the cell is used to it. So far, none of these mutations has troubled this cell.
And then, one day, it happens.
Purely by chance, a toxin, perhaps a component of tobacco that makes the substance so deadly, finds its way deep into regions of the cell’s nucleus and damages what’s called an oncogene, a class of normal genes that, when mutated, cause a cell to grow out of control. Weinberg, who identified the first human oncogene in 1982, compares the effect of a damaged oncogene to a gas pedal stuck to the floor. And that is why this cell, although oblivious to any of the other mutations it has experienced in the past, notices this one.
The equilibrium in the tissue is disturbed. The cell divides, and divides again, but this time not in response to another cell’s death. It copies itself at will. When it divides, each new clone retains the ability to divide, unprompted, on its own. And so on. But this new genetic twist affords only that particular cell and its progeny limited unfettered reproduction. The cell is held in check by a tumor suppressor gene, another class of genes that acts as a sort of emergency brake system to slow down the effect of this stuck pedal. With tumor suppressor genes acting vigilantly, this micro-cluster of a few extra cells is harmless. The tumor suppressors create a firewall that prevents the cell from growing out of control.
The cell and its small cohort remain in this state for years, until one day a new toxin defeats seemingly insurmountable odds and disables a single tumor suppressor gene in this small cell cluster. Now, gas pedal stuck, brake system disabled, the cell division picks up speed. Gradually, a small and irregular—and, at this point, still inoffensive—gathering of cells takes shape.
The tissue that houses this cluster has seen this sort of thing before. Over the years, other tiny groups if cells have experienced similar mutations and started to grow at random. “In a sense, our bodies are constantly developing microscopic pre-cancerous growths,” says Tan Ince, a scientist in Weinberg’s lab and pathologist at Brigham and Women’s Hospital in Boston. “It’s just that 99.999 percent of the time, the body is able to take care of them.”
The body does this by using a group of proteins whose sole purpose is to maintain cell-growth equilibrium within the tissue. When a cell starts growing out of synch with its neighbors, the tissue sends these proteins to the cells instructing them to stop. Some cells, as a result, never grow again; others are only temporarily held at bay.
This cluster of a few thousand cells, which is still benign, receives these anti-growth signals and obediently stops in its tracks. For the tumor, that’s just fine. After all, it’s only following the dictates of both its internal and environmental biology, and when it’s told to stop, it stops. And this tumor isn’t alone. Others like it have been stopped at this particular stage, never to grow again—and we are none the wiser.
Of course, toxins from a variety of sources—environment, food, chemical substances—continue to travel through the tissue. Some even cause more mutations in this microscopic tumor, but in every case, the mutations occur in areas that don’t affect its behavior. A few of the cells in the tumor still are able to divide, a process that can cause slight mutations. But again, like most mutations resulting from cell division, nothing happens. And the tumor remains in this state for years, perhaps even a decade or more.
Eventually, a random toxin finds its way through the tumor and mutates a single gene in a cell inside the mass. This time, the damaged gene happens to be a critical node in the cell’s network through which it processes the anti-growth signals that have been keeping it in check.
“Think of it as the World Wide Web,” says Ince. “You can hit any number of nodes in the network, and it won’t be a problem. But then you hit one that has a ripple effect and it brings the whole network down.”
That one cell, embedded deep within the tumor, already with oncogene and tumor suppressor gene damaged, is now deaf to anti-growth messages. The network isn’t working as it should. It begins dividing again, creating clones which, in turn, contain these same mutations.
Then, a roadblock: Orders from the host tissue instruct individual cells in the tumor to kill themselves. A succession of mass suicides begins. The tumor does nothing to stop it.
The sacrificial cell
Biologists call this apoptosis—also known as programmed cell death. The process, named by British biologist Andrew Wyllie in 1972, refers to the ancient Greek term for leaves falling from a tree. In the cell, however, the process isn’t nearly as pastoral as the changing of seasons. Proteins on the cell surface receive these suicide orders and deliver them to other proteins deep within the cell. Additional signals may even originate within the cell itself. The message continues, protein to protein, via an intricate network that converges on the mitochondria, a group of cellular internal organs whose responsibilities include, among other things, turning food into energy. These mitochondria release a chemical catalyst that launches the suicide process. The cell membrane begins to crumble, the chromosomes degrade, the nucleus fractures, and within the space of a few hours the cell is a microscopic cadaver, swallowed up by nearby cells.
It very well could all end here. The growth rate of the tumor has been significantly curbed by the scores of cells sacrificing themselves for the greater good of the organism. While the tumor won’t disappear as a result, it can stop growing altogether.
“Scientists are researching new forms of therapy designed to induce cancer cells to enter apoptosis,” says Weinberg, noting the effectiveness of this natural process. Drugs that target this process in tumor cells while sparing healthy cells, however, still are in early developmental stages.
It’s not easy to coax a cell into killing itself. The entire process is complex and many proteins need to be recruited for it to work. But there is one star player, a gene called p53. This gene was first discovered by Princeton University biologist Arnold Levine in 1979, but it wasn’t until the late 1990s that Levine and other researchers realized it was a critical component in this suicide network. p53, along with the protein it produces, assesses the health of a cell and its genome and, when necessary, acts as a conduit through which signals reach the suicide machinery.
But somewhere inside the tumor, a single cell that has not yet received its suicide order divides, and in doing so introduces a mutation that disrupts its p53 gene, a mutation that is found in more than half of all human cancers. With p53 damaged, the new cell produced by this division contains a suicide network in disarray. A suicide order enters the cell, but the passing of information breaks down and never reaches the mitochondria. And when this cell then divides and divides again (its hyperactive oncogene continually pushing for more rapid cell divisions) the tumor will enter a new phase as all of its progeny quickly form a new clump of cells, each containing disabled suicide networks.
It’s important to remember that in spite of how far this fledgling tumor has come, it really isn’t any “smarter” than when it started. Each new capability it gains is the result of a series of random mutations. “There’s no ‘learning’ going on here,” says Bert Vogelstein, professor at the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins. “The tumor isn’t developing any new skills. This is all chance. In macro-evolution, organisms don’t learn anything, they’re just selected. Here it’s the same thing on the cellular level.”
Evolution may have rejuvenated this tumor’s reproductive power, but the tumor, like all other organisms, can’t live forever. Its ability to grow apart from what its environment dictates is trumped by an internal machinery that is programmed for a specific amount of cellular division. Even the most mutated cell eventually enters into its golden years, and when it finally reaches its division quota, quietly passes on.
Forbidden fruit
The original lineage of cells that triggered the tumor growth is gone. Since typical human cells divide anywhere from 60 to 70 times—sometimes once a day, and other times once a month or even once a year—we can then assume that this cell and its daughter cells passed on some time ago. That’s because cells possess an internal clock controlled by something called the “telomere,” a region of DNA that lives at the endpoints of each of the 46 chromosomes. The telomere preserves the chromosomes, but with each cell division, the new cells lose some of this region, until eventually this protective shield is gone altogether—a process that James Watson, co-discoverer of DNA’s double helix, predicted in 1972. And so, when the original cell divided into two daughter cells, and those two resulting cells subsequently divided, each new cell contained less of the telomere than its predecessor. And so on.
“Certain cells, such as sperm or stem cells, contain an enzyme that preserves the telomere through each cell division and as a result, these cells become ‘immortal’,” able to replicate endlessly without any limitation, says Douglas Hanahan, a professor of biochemistry at University of California, San Francisco. All cells in the body contain the gene that creates this telomere-producing enzyme, but with the exception of sperm cells and stem cells, it is inaccessible. Weinberg describes this gene as the genetic “apple from the Tree of Knowledge, forbidden to most normal cells in the body.”
However, through a process that researchers don’t fully understand, the tumor breaches this mortality barrier. In some tumors this happens early on; with others it’s later. But somehow, a group of cells manages to activate this “forbidden” gene, starting the production of that immortality-giving enzyme. With each subsequent cell division, the telomere remains intact, and so the cells divide 70, 100, 140 times, each time passing on perpetual youth to their cellular offspring.
Because almost all types of cancer possess this ability to replicate unchecked, disabling the process is a tempting target for drug makers. “Attempts to make telomerase inhibitors that could shut down the enzyme are attractive in principle,” says Weinberg, “but have, until now, proven difficult.”
For now, this tumor, which has transformed itself over the years from a simple collection of otherwise normal-looking cells to a tissue with its own uniquely abnormal architecture, has achieved an immortality of sorts.
Tripping the malignant switch
Even though it has evolved beyond so many of its environmental constraints, and despite its gradually mounting size, the tumor remains benign. It may have grown resistant to the host tissue’s attempts to restrain it but, ultimately, the tumor still needs the tissue to live. The tumor requires a steady supply of blood to grow, and although it has siphoned blood from the host, the lack of its own vascular network keeps it in a relatively immature state.
But over the life of the tumor, a slow and steady process innate to the body’s immune system has gained momentum. Early in this particular tumor’s development, when it was no more than a small lesion, the immune system detected it, but misdiagnosed it as a wound. The immune system’s primary healing response is to enable a wound to grow blood vessels—a process known as angiogenesis.
“Remember,” says Hanahan, “the immune system isn’t smart enough to say, ‘Hey, that’s cancer!’ It hasn’t evolved to the point where it recognizes cancer as an enemy.” Instead, it looks for foreign invaders like viruses and bacteria. The immune system, mistaking the identity of the tumor, feeds it with proteins that spawn a vascular network. “It can literally bathe the cells with these angiogenic growth factors,” says Hanahan.
Slowly, over many years, scores of small capillaries have developed, some growing into larger, more robust blood vessels. Eventually, the vessels reach maturity, and now, with the blood flowing freely and abundantly, the tumor has become a self-contained system, a sort of organ within an organ. With no constraints, and wholly independent, it continues to grow.
Few areas of tumor development have gained as much attention in recent years as angiogenesis. Unlike research on apoptosis or telomere, angiogenesis is one area in which scientists have experienced success in drug trials. Harvard University scientist Judah Folkman, who often collaborates with Hanahan, has developed drugs that block these growth-factor proteins, one of which received approval from the Food and Drug Administration in February. “It’s too early to tell just how successful these therapies will be,” Hanahan says, “but the early signs are promising.”
At this stage of the tumor’s development, it has remained within the confines of particular tissue membranes, contained by a sheath of proteins that prevent it from invading other areas of the organ housing it. Therefore, if a physician were to remove or destroy it, the patient could be assured that all traces of the cancer are gone and that there will be no recurrence whatsoever.
But as the tumor grows, its sheer size becomes a threat. For many years it has been slowly chafing away at this inner sheath of proteins that has enveloped it since its inception, generating enzymes that slowly eat away at this layer. As it expands, it degrades the shield, and eventually, the tissue tears. A small section of the tumor works its way into this tiny perforation. More enzymes deepen the wound. The tumor expands, the tear increases, and the tumor breaks through this layer, gaining access to tissues in the organ that before were inaccessible.
Like many of these stages of tumor development, this can happen early, or, as this example describes, at a later stage. But either way, “the malignant switch has finally been tripped,” says Weinberg. “At this point the tumor can invade anywhere it wants in the body. Breaking through this tissue layer is a harbinger of its ability to invade in more distant sites and trigger metastasis.”
The final frontier
Now, were a surgeon to remove the tumor or destroy it with a few blasts of radiation, there is no certainty that the patient would recover: Since the tumor broke through that protective protein layer and made its way deeper into the tissue, it is no longer bound to any particular location. Now it has full access to the inner workings of the organ in which it’s been living for so many decades, including the vascular networks that branch throughout the entire body. The tumor begins to scatter individual cancer cells into the bloodstream, in much the same way that a plant scatters its seeds to the four winds. The original tumor can be destroyed, but the vagrant seeds cannot be gathered.
Yet just as few plant seeds find fertile soil, the cells scattered by this tumor will find few, if any, areas in the body hospitable to them. These cells have evolved to bypass all the body’s strategies for curbing their growth, but they have developed these capabilities within the context of a single organ tissue. Weinberg sees these cells less like an army that sweeps through foreign lands conquering and pillaging and more like the first pilgrims who landed on American soil and were nearly devastated by their first New England winter. The tragedy of the pilgrims is that almost half died; the tragedy of the cancer cells is that one or two out of millions manage to survive.
When the tumor cells leak into the bloodstream, many die there. Even those that survive don’t have an easy time. “Exhausted by the rigors of the voyage,” says Weinberg, “a few remaining cells finally land in new organ tissues and are assaulted right away by a brand new biochemical milieu.”
However, in one region of the body that has vanquished just about every cancer cell that tried to settle there, one cell survives. The process of evolution that occurred so long ago, initiating the formation of the first tumor, begins again in this single cell. Because the cell inherited the immune system-defeating mutations from the original tumor, it matures at an accelerated rate. It, too, soon will become a tumor, and at some point, it will send cells into the bloodstream to settle in distant sites. And because the primary tumor may have gone unnoticed, this secondary tumor may be the patient’s first indication that something is wrong.
On a molecular level, this process, called metastasis, is poorly understood. “It’s really the last great frontier in cancer research in the sense that we really don’t understand how the primary tumors succeed in dispatching cells to distant sites, and how they succeed then in creating new colonies of tumor cells,” says Weinberg. “This is a complex issue that we barely understand at present.”
For the moment, there are far more questions than answers. Do tumors acquire the ability to metastasize, or do they draw upon an existing store of information housed in their genomes? Are there specific genes that enable a cell to become invasive or metastatic, the equivalent to oncogenes and tumor suppressor genes? What exactly is it that enables, or prevents, wandering cancer cells from successfully founding new colonies at distant sites? “Right now it’s a pretty wide open field, and there are many competing theories,” Weinberg observes. “There’s an enormous amount of data but little conceptual clarity.”
Today, Weinberg’s lab at Whitehead is focusing on five genes involved in early embryonic development, genes colorfully named Slug, Snail, Goosecoid, Twist, and Mesenchyme forkhead after the bizarre embryos that their mutated forms can cause in flies. Weinberg is exploring the hypothesis that tumors opportunistically resurrect these genes and use them to acquire traits for metastasis and invasiveness.
While this theory hasn’t yet been fully demonstrated, scientists know that once the tumor has acquired these abilities, it is profoundly difficult to control. “It’s always an uphill battle for the tumor,” says Ince. “Now, though, it has everything it needs to keep marching on.”
The original tumor and its progeny are by no means invincible. Doctors soon will know the full extent of the disease. The original tumor and the obvious secondary tumors will be destroyed. A few cells likely will escape these treatments and seek refuge deeper in the tissue or the bloodstream, only to be poisoned by a flood of chemotherapy. Fledgling tumors might starve to death from the newer therapies that choke off their ability to grow blood vessels. Or, some tumors might experience therapeutic assaults specially designed for them alone, thanks to recent advances in genetic profiling.
But even the most aggressive treatments can leave a single, lone cancer cell unscathed. Once again, everything will depend upon the unpredictable outcome of natural selection. That cell can thrive, or it can die, or it can form a kind of tumor that the body constrains for the rest of the patient’s life. No one knows.
The ending of this tumor’s biography is, for now, uncertain. Evolution has no favorites, and that’s both a blessing and a curse.
Topics
Contact
Communications and Public Affairs
Phone: 617-452-4630
Email: newsroom@wi.mit.edu