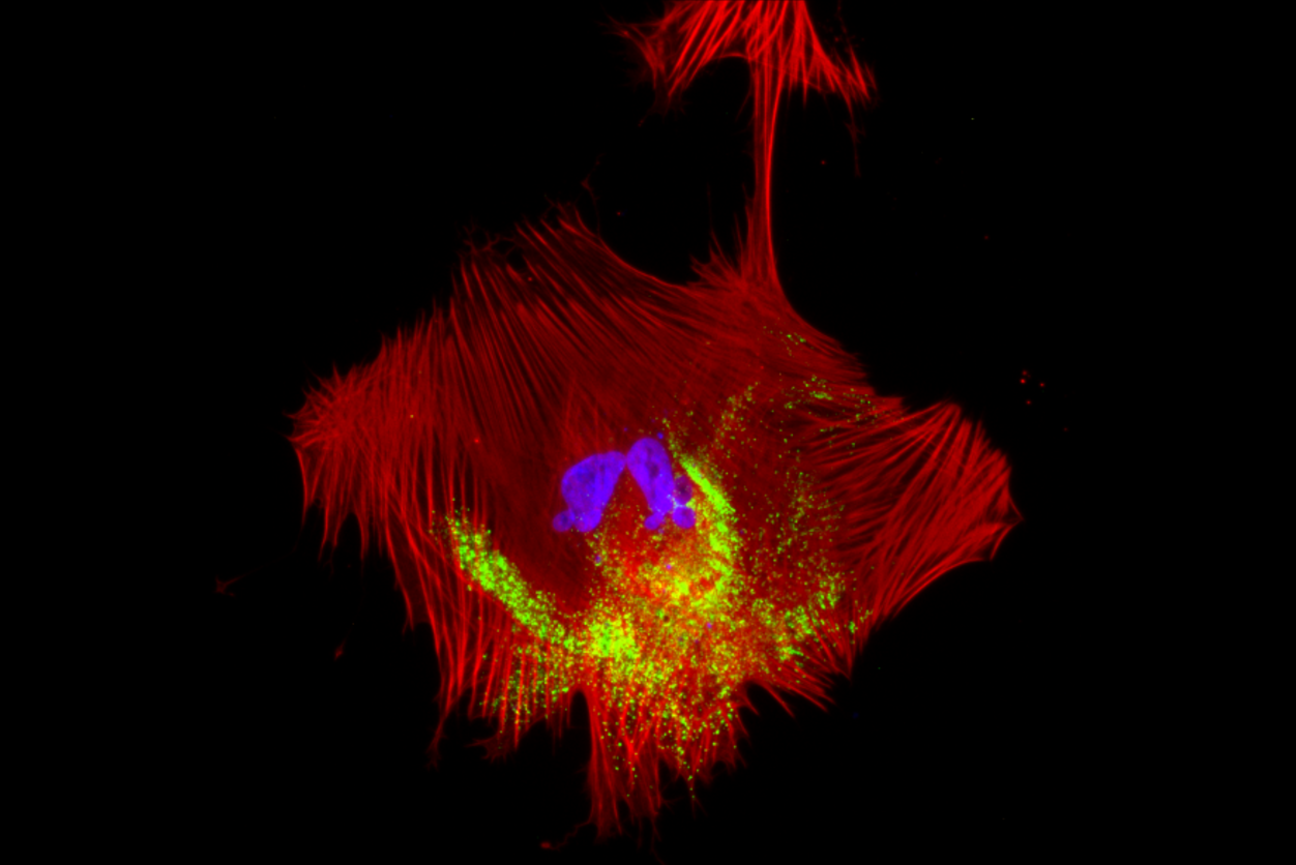
A human pluripotent stem cell-derived smooth muscle cell infected with the virus SARS-Cov-2. Sites of viral genome replication are in green.
Alexsia Richards/Whitehead Institute
Cellular interactions help explain vascular complications due to COVID-19 virus infection
COVID-19 is a respiratory disease primarily affecting the lungs. However, the SARS-CoV-2 virus that causes COVID-19 surprised doctors and scientists by triggering an unusually large percentage of patients to experience vascular complications – issues related to blood flow, such as blood clots, heart attacks, and strokes.
Whitehead Institute Founding Member Rudolf Jaenisch and colleagues wanted to understand how this respiratory virus could have such significant vascular effects. They used pluripotent stem cells to generate three relevant vascular and perivascular cell types—cells that surround and help maintain blood vessels—so they could closely observe the effects of SARS-CoV-2 on the cells. Instead of using existing methods to generate the cells, the researchers developed a new approach, providing them with fresh insights into the mechanisms by which the virus causes vascular problems. The researchers found that SARS-CoV-2 primarily infects perivascular cells and that signals from these infected cells are sufficient to cause dysfunction in neighboring vascular cells, even when the vascular cells are not themselves infected. In a paper published in the journal Nature Communications on December 30, Jaenisch, postdoc in his lab Alexsia Richards, Harvard University Professor and Wyss Institute for Biologically Inspired Engineering Member David Mooney, and then-postdoc in the Jaenisch and Mooney labs Andrew Khalil share their findings and present a scalable stem cell-derived model system with which to study vascular cell biology and test medical therapies.
A new problem requires a new approach
When the COVID-19 pandemic began, Richards, a virologist, quickly pivoted her focus to SARS-CoV-2. Khalil, a bioengineer, had already been working on a new approach to generate vascular cells. The researchers realized that a collaboration could provide Richards with the research tool she needed and Khalil with an important research question to which his tool could be applied.
The three cell types that Khalil’s approach generated were endothelial cells, the vascular cells that form the lining of blood vessels; and smooth muscle cells and pericytes, perivascular cells that surround blood vessels and provide them with structure and maintenance, among other functions. Khalil’s biggest innovation was to generate all three cell types in the same media—the mixture of nutrients and signaling molecules in which stem cell-derived cells are grown.
The combination of signals in the media determines the final cell type into which a stem cell will mature, so it is much easier to grow each cell type separately in specially tailored media than to find a mixture that works for all three. Typically, Richards explains, virologists will generate a desired cell type using the easiest method, which means growing each cell type and then observing the effects of viral infection on it in isolation. However, this approach can limit results in several ways. Firstly, it can make it challenging to distinguish the differences in how cell types react to a virus from the differences caused by the cells being grown in different media.
“By making these cells under identical conditions, we could see in much higher resolution the effects of the virus on these different cell populations, and that was essential in order to form a strong hypothesis of the mechanisms of vascular symptom risk and progression,” Khalil says.
Secondly, infecting isolated cell types with a virus does not accurately represent what happens in the body, where cells are in constant communication as they react to viral exposure. Indeed, Richards’ and Khalil’s work ultimately revealed that the communication between infected and uninfected cell types plays a critical role in the vascular effects of COVID-19.
“The field of virology often overlooks the importance of considering how cells influence other cells and designing models to reflect that,” Richards says. “Cells do not get infected in isolation, and the value of our model is that it allows us to observe what’s happening between cells during infection.”
Viral infection of smooth muscle cells has broader, indirect effects
When the researchers exposed their cells to SARS-CoV-2, the smooth muscle cells and pericytes became infected—the former at especially high levels, and this infection resulted in strong inflammatory gene expression—but the endothelial cells resisted infection. Endothelial cells did show some response to viral exposure, likely due to interactions with proteins on the virus’ surface. Typically, endothelial cells press tightly together to form a firm barrier that keeps blood inside of blood vessels and prevents viruses from getting out. When exposed to SARS-CoV-2, the junctions between endothelial cells appeared to weaken slightly. The cells also had increased levels of reactive oxygen species, which are damaging byproducts of certain cellular processes.
However, big changes in endothelial cells only occurred after the cells were exposed to infected smooth muscle cells. This triggered high levels of inflammatory signaling within the endothelial cells. It led to changes in the expression of many genes relevant to immune response. Some of the genes affected were involved in coagulation pathways, which thicken blood and so can cause blood clots and related vascular events. The junctions between endothelial cells experienced much more significant weakening after exposure to infected smooth muscle cells, which would lead to blood leakage and viral spread. All of these changes occurred without SARS-CoV-2 ever infecting the endothelial cells.
This work shows that viral infection of smooth muscle cells, and their resultant signaling to endothelial cells, is the lynchpin in the vascular damage caused by SARS-CoV-2. This would not have been apparent if the researchers had not been able to observe the cells interacting with each other.
Clinical relevance of stem cell results
The effects that the researchers observed were consistent with patient data. Some of the genes whose expression changed in their stem cell-derived model had been identified as markers of high risk for vascular complications in COVID-19 patients with severe infections. Additionally, the researchers found that a later strain of SARS-CoV-2, an Omicron variant, had much weaker effects on the vascular and perivascular cells than did the original viral strain. This is consistent with the reduced levels of vascular complications seen in COVID-19 patients infected with recent strains.
Having identified smooth muscle cells as the main site of SARS-Cov-2 infection in the vascular system, the researchers next used their model system to test one drug’s ability to prevent infection of smooth muscle cells. They found that the drug, N, N-Dimethyl-D-erythro-sphingosine, could reduce infection of the cell type without harming smooth muscle or endothelial cells. Although preventing vascular complications of COVID-19 is not as pressing a need with current viral strains, the researchers see this experiment as proof that their stem cell model could be used for future drug development. New coronaviruses and other pathogens are frequently evolving, and when a future virus causes vascular complications, this model could be used to quickly test drugs to find potential therapies while the need is still high. The model system could also be used to answer other questions about vascular cells, how these cells interact, and how they respond to viruses.
“By integrating bioengineering strategies into the analysis of a fundamental question in viral pathology, we addressed important practical challenges in modeling human disease in culture and gained new insights into SARS-CoV-2 infection,” Mooney says.
“Our interdisciplinary approach allowed us to develop an improved stem cell model for infection of the vasculature,” says Jaenisch, who is also a professor of biology at the Massachusetts Institute of Technology. “Our lab is already applying this model to other questions of interest, and we hope that it can be a valuable tool for other researchers.”
Richards, A., Khalil, A.S., Friesen, M. et al. SARS-CoV-2 infection of human pluripotent stem cell-derived vascular cells reveals smooth muscle cells as key mediators of vascular pathology during infection. Nat Commun 15, 10754 (2024). https://doi.org/10.1038/s41467-024-54917-4
Topics
Contact
Communications and Public Affairs
Phone: 617-452-4630
Email: newsroom@wi.mit.edu


