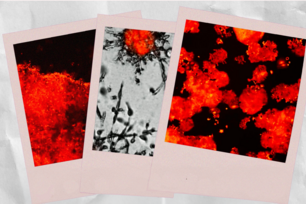
Researchers discovered that a low-dose HSP90 inhibitor combined with an anti-estrogen agent impedes the cell cycle, thereby thwarting replication of tumor cells and limiting the introduction of adaptive (i.e., drug-resistant) mutations. The images at left depict tumor tissue from a mouse model of breast cancer. Brown staining indicates significant levels of levels of phosphorylated retinoblastoma protein (Phospho-RB), which is a marker of cell cycle progression. Image A displays untreated tissue, while images B and C show the tissue treated with the anti-estrogen drug tamoxifen and an HSP90 inhibitor, respectively. The tissue in image D, treated with a combination of tamoxifen and an HSP90 inhibitor, displays a dramatic reduction in Phospho-RB, signaling a halt in tumor-cell replication.
Courtesy of PNAS
Heat-shock protein enables tumor evolution and drug resistance in breast cancer
CAMBRIDGE, Mass. – Long known for its ability to help organisms successfully adapt to environmentally stressful conditions, the highly conserved molecular chaperone heat-shock protein 90 (HSP90) also enables estrogen receptor-positive (ER+) breast cancers to develop resistance to hormonal therapy.
This HSP90-mediated evolutionary mechanism of drug resistance, reported by Whitehead Institute scientists in this week’s online edition of the Proceedings of the National Academy of Sciences (PNAS), provides a strong therapeutic rationale for combining HSP90 inhibition with other interventions not only in the treatment of ER+ breast cancers but in other tumor types as well.
HSP90’s role in the emergence of beneficial heritable traits in organisms ranging from yeast to vertebrates has been an area of intense focus for Whitehead Member Susan Lindquist’s lab. Several years ago, her lab found that HSP90 enables disease-causing fungi to evolve resistance to today’s antifungal medications. Follow-on studies showed that an HSP90 inhibitor combined with a conventional antifungal could be effective against drug-resistant isolates of the pathogenic fungi Candida albicans and Aspergillus fumigatus, both capable of causing lethal infections, particularly in immunocompromised patients.
Based on this work, lab members wondered whether a similar dynamic might be at play in malignant tumors; in particular, ER+ breast cancers, whose growth is fueled by the hormone estrogen. ER+ breast cancer, the most common breast cancer subtype, is treated with hormonal therapies that either block the estrogen receptor or thwart the production of estrogen. Though responsive to hormonal therapy at first, the tumors in almost all patients with metastatic disease at the time they are diagnosed become drug resistant. Now it’s clear that HSP90 contributes to such resistance by enabling tumors to adapt to the severe stress caused by depriving them of the support that the hormone normally provides.
“Here, you take away the growth factor, in this case estrogen, that the tumor cells depend on, and HSP90 enables alternate growth pathways,” says Luke Whitesell, a clinical oncologist and scientist in the Lindquist lab. “It’s a bit like a game of whack-a-mole, where you knock down estrogen and up pops another growth promoter.”
In a series of experiments, Whitesell—who is the first author of the PNAS paper—and colleagues found that in both in vitro and in vivo models of ER+ breast cancer, the addition of an HSP90 inhibitor (even at very low levels that had no effect on their own) to an anti-estrogen agent was sufficient to prevent development of resistance to the anti-estrogen. Mechanistically, the researchers found that HSP90 inhibition increases the ability of the anti-estrogen to block the cell cycle, thereby thwarting the replication of tumor cells.
“At the end of the day, what we do see in cell culture and in animals is a profound cell cycle block, which we would expect to limit the accumulation of adaptive mutations,” Whitesell says.
“These exciting results provide a strong rationale to explore the effect of HSP90 inhibitors when added to hormonal therapy for ER-positive breast cancer,” says Nancy Lin, the Clinical Director of the Breast Oncology Center at Dana-Farber Cancer Institute and Assistant Professor at Harvard Medical School.
Lin is serving as principal investigator of an active clinical trial in which patients with recurrent or metastatic ER+ breast cancer are being treated either with the hormonal therapy fulvestrant, currently marketed by AstraZeneca as Faslodex, or with a combination of fulvestrant and ganetespib, an HSP90 inhibitor being developed by Synta Pharmaceuticals.
“The study is actively recruiting patients, and we hope to have results within the next several years,” adds Lin.
Whitesell notes that, independent of the current trial’s results, HSP90’s role in the evolution of drug resistance in cancers warrants further exploration. In fact, he argues that administering HSP90 inhibitors at low dose in ways unique from those in which they’ve been investigated thus far could prove beneficial in preventing the rapid emergence of resistance that has drastically compromised the effectiveness of the newest targeted therapies for melanoma, non-small cell lung cancer, and the brain cancer glioblastoma.
This work was supported by the National Institutes of Health (grant K08NS064168), the National Cancer Institute (grant K99CA175293), the Susan G. Komen Foundation (grant KG110450), and Howard Hughes Medical Institute.
* * *
Susan Lindquist’s primary affiliation is with Whitehead Institute for Biomedical Research, where her laboratory is located and all her research is conducted. She is also a Howard Hughes Medical Institute investigator and a professor of biology at Massachusetts Institute of Technology.
* * *
Citation:
Whitesell, L., Santagata, S., Mendillo, M. L., Lin, N. U., Proia, D. A., & Lindquist, S. (2014). HSP90 empowers evolution of resistance to hormonal therapy in human breast cancer models. Proceedings of the National Academy of Sciences, 111(51), 18297-18302. doi:10.1073/pnas.1421323111
Topics
Contact
Communications and Public Affairs
Phone: 617-452-4630
Email: newsroom@wi.mit.edu