Signaling pathways point to vulnerability in breast cancer stem cells
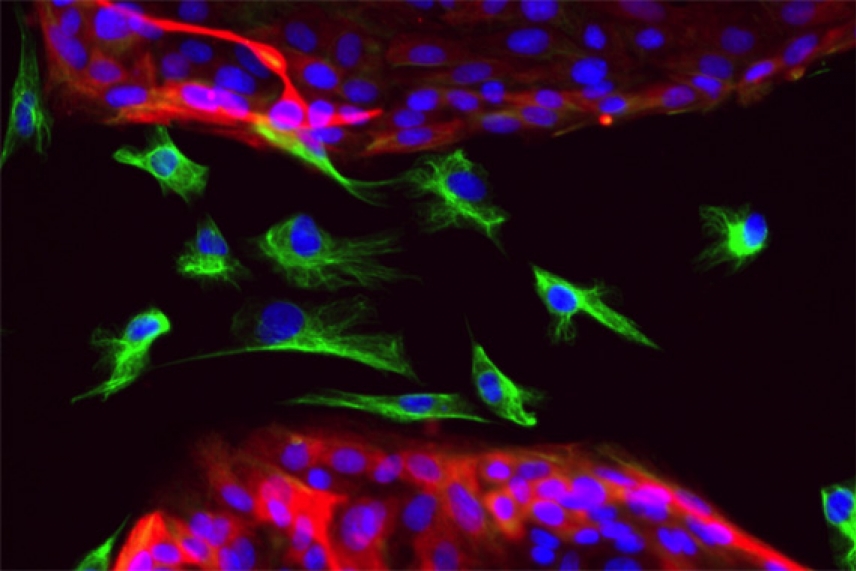
Epithelial and mesenchymal cells
Christina Scheel/Whitehead Institute
CAMBRIDGE, Mass. – Whitehead Institute researchers have identified signals from breast epithelial cells that can induce those cells to transition to and maintain a mesenchymal and stem cell-like cell state that imbues both normal and cancer cells with a greater ability to migrate and self-renew. Interrupting these signals strips the cells of the migratory, invasive and self-renewal abilities used by cancer stem cells to seed new tumors.
"Stem cells are important in both cancers and normal tissues. On the one hand we'd like to know what creates so-called cancer stem cells in tumors and on the other hand we'd like to know what creates normal stem cells in normal epithelial tissues," says Whitehead Founding Member Robert Weinberg. "We have reason to believe that these two dynamics are orchestrated by a common regulatory machinery. So this work may be applicable for understanding both breast cancer cells and normal epithelial cells, such as the normal cells in the normal mammary ducts."
During an epithelial-to-mesenchymal transition (EMT), epithelial cells acquire the traits of mesenchymal cells. Unlike the tightly-packed epithelial cells that stick to one another, mesenchymal cells are loose and free to move around a tissue. The attributes of mesenchymal cells are beneficial during development, but when hijacked by cancer cells, confer the ability to migrate to distant sites. In addition, the passage through an EMT enables adult cancer cells to seed new tumors with high efficiency, the hallmark trait of cancer stem cells. Although passage through an EMT is recognized as an important step in the formation of cancer stem cells, scientists have been unable to clearly identify the cues in a cell's microenvironment that induce an EMT.
By studying human breast epithelial cells, Christina Scheel, a postdoctoral researcher in the Weinberg lab, pinpointed three signaling pathways (TGF-beta, non-canonical Wnts, and canonical Wnts) that work together to maintain migratory and self-renewing traits of both normal breast epithelial and breast cancer cells. These pathways are continuously activated in the stem cells by autocrine signals; that is, signals produced by the cells themselves. Studying how these autocrine signals function in breast epithelial cells allowed Scheel to specify the signals that allow these cells to pass through an EMT and enter into a mesenchymal and stem cell-like state in the first place. Her findings are published in the June 10 issue of Cell.
Interestingly, Scheel discovered that epithelial cells are kept in their differentiation state via inhibition of the three signaling pathways, that is, normal epithelial cells naturally produce proteins that block these signaling proteins. To push normal breast epithelial cells through an EMT in vitro, she removed these endogenous inhibitors by administering a cocktail of neutralizing antibodies and added growth factors that stimulate the three pathways, thereby mimicking the autocrine signaling found in mesenchymal cells. By applying the resulting EMT-inducing cocktail continuously, Scheel pushed the cells into a mesenchymal and stem cell-like state, with associated increased migratory ability and stem cell-like characteristics. Eventually, the former epithelial cells stabilized this state through autocrine signaling and were no longer dependent on the EMT cocktail.
To see the effects of blocking this autocrine signaling in an animal model, Scheel implanted into mice human breast cancer epithelial cells that had passed through an EMT. She then injected the implantation site with proteins that block the three pathways. The injected mice had one-tenth the number of tumors found in mice that did not receive the inhibitory proteins. In addition, breast cancer cells that were pre-treated in vitro with these proteins displayed a greatly reduced ability to metastasize when subsequently implanted into mice.
Scheel notes that these experiments show how cancer cells' knack for usurping normal cell functions could ultimately lead to their downfall.
"These autocrine signals are not something breast cancer cells invent anew, but derive instead an activation of normal stem cell programs," says Scheel. "Breast cancer stem cells rely on these signals to maintain themselves, so they remain susceptible to blocking this autocrine signaling. It might be a terrific way to target breast cancer stem cells. In addition, our gain in understanding how both migratory and self-renewal traits are activated in normal breast epithelial cells might further our understanding of normal tissue homeostasis and might be of great utility in the area of regenerative medicine, where it would be highly desirable to create great numbers of epithelial stem cells without resorting to genetic intervention."
Although Scheel's research gives new insight into how both cancer and normal breast cells transition to and maintain a mesenchymal cell state, she and Weinberg caution that the same signals and signaling pathways may not apply for non-breast cells.
"Are the same agents signaling the EMT in non-mammary tissues – the skin, liver, the gut, pancreas and so forth? We don't know the generalizability of Scheel's findings yet, although I can imagine that there are many commonalities," says Weinberg, who is also a professor of biology at MIT and the Director of the MIT/Ludwig Center for Molecular Oncology. "Secondly, we don't know if these three signaling pathways are ultimately those that are critically important for activating the EMT in non-mammary cell types. Alternatively, there may be other contextual signals besides these three that play an equally important role in triggering an EMT in non-mammary cells? Whether these signaling pathways turn out to have a degree of universality, we just don't know."
This research was supported by the National Institutes of Health/National Cancer Institute (NIH/NCI), Massachusetts Institute of Technology Ludwig Center for Molecular Oncology, Ludwig Fellowship for Metastasis Research, Breast Cancer Research Foundation, Harvard Breast Cancer Specialized Program of Research Excellence (SPORE), Department of Defense Breast Cancer Research Program Idea Award, and Samuel Waxman Foundation.
* * *
Robert Weinberg’s primary affiliation is with Whitehead Institute for Biomedical Research, where his laboratory is located and all his research is conducted. He is also a professor of biology at Massachusetts Institute of Technology and Director of the MIT/Ludwig Center for Molecular Oncology.
* * *
Citation:
Scheel, C., Eaton, E. N., Li, S. H. J., Chaffer, C. L., Reinhardt, F., Kah, K. J., ... & Weinberg, R. A. (2011). Paracrine and autocrine signals induce and maintain mesenchymal and stem cell states in the breast. Cell, 145(6), 926-940.
Topics
Contact
Communications and Public Affairs
Phone: 617-452-4630
Email: newsroom@wi.mit.edu