Screening Technique Streamlines Search for Anticancer Drug
CAMBRIDGE, Mass. — Most cancer patients face an all or nothing dilemma. Aggressive chemotherapy can and often does kill cancerous cells, shrink tumors and increase a patient’s chance for survival. But chemo’s toxic chemicals kill healthy cells too, causing severe side effects like anemia, organ damage and even memory loss.
In a study reported in the March 24 issue of Cancer Cell, researchers detail an approach to rapidly identify chemical compounds that are active only in the presence of certain cancer-causing genes and proteins—a step toward finding drugs that are lethal only to cancer cells. This strategy, which pairs chemical compounds with the specific genetic mutations they are likely to react against, also opens the door to a new way to custom-tailor chemotherapy.
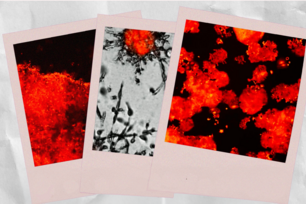
Brent Stockwell and his colleagues at Whitehead Institute for Biomedical Research in Cambridge, Mass., used a novel screening technique to survey more than 23,000 chemical compounds and test for their ability to kill human cancer cells. In particular, Stockwell mined this “chemical library” for compounds that killed cancer cells while leaving healthy cells unharmed. The group identified nine compounds matching this profile, including one previously unidentified compound that seems to kill cancer cells through a different mechanism than many conventional cancer drugs.
High-throughput, Quick Results
Over the last decade, researchers have identified some of the genes and proteins most commonly implicated in the cascade of cellular events leading to cancer. In this study, Stockwell used human cancer cells engineered to contain a selection of these common genetic aberrations, including the ras and htert oncogenes and two known oncoproteins (proteins implicated in cancer development).
The lab developed a screening assay that exposed the engineered cancer cells to a barrage of chemical tests. Results of these tests were fed into a database that tracked the results and scored the compounds based on their effectiveness. Ultimately, the screen whittled down the field of 23,000 compounds to find those that were active only in the presence of the cancer-causing genes and proteins.
“Using this system, we searched for compounds that become active only in the presence of commonly mutated genes,” says Stockwell. “We’ve identified several compounds, including one previously unknown compound, that had exactly the effect we were looking for.”
Mass screening like this—what scientists call high-throughput testing—represents a new and emerging paradigm in drug discovery. “The old method to find drug candidates was to take tumor cells from a human tumor, and find things that killed them, without really understanding how they would ultimately affect other cells in the body,” Stockwell explains. “Drug candidates identified by this method often turned out to be completely toxic to healthy cells and thus, not usable as a therapy.”
In addition to investigating its therapeutic implications, Stockwell and his colleagues are using this screening technique to study the cell signaling pathways driving tumor growth.
Erastin
Of the compounds Stockwell’s team identified, four are currently used in clinical practice to treat tumors. A better understanding of how these drugs work may offer vital insight into which drugs are more likely to be effective against a particular type of cancer. “We discovered that these anticancer drugs are particularly effective in tumor cells with specific genetic changes, suggesting a strategy by which we can tailor the use of these drugs to fit a patient’s unique tumor type,” says Stockwell.
One of the compounds found to be more potent in the presence of the cancer-linked genetic aberrations has never been studied nor its potential as an anti-cancer drug explored. Stockwell’s group currently is conducting follow-up studies to determine how this unique compound, which they named erastin, works.
Erastin is especially interesting to researchers because it seems to kill cancer cells differently than many drugs on the market. Instead of inducing cell death as do many cancer drugs—a process known as apoptosis—erastin seems to kill the cancer cell by an unknown mechanism.
“The most immediate thing is to figure out how erastin works and try to understand that molecular mechanism in detail,” Stockwell added.
The engineered cancer cells used in this study were created by William Hahn and Stephen Lessnick at Dana Farber Cancer Institute. The study was funded in part by the National Cancer Institute and the Burroughs Wellcome Fund.
Citation
Dolma, S., Lessnick, S. L., Hahn, W. C., & Stockwell, B. R. (2003). Identification of genotype-selective antitumor agents using synthetic lethal chemical screening in engineered human tumor cells. Cancer cell, 3(3), 285-296.
Topics
Contact
Communications and Public Affairs
Phone: 617-452-4630
Email: newsroom@wi.mit.edu